Abstract
Background: Management of CML with TKIs is constrained by treatment resistance, which portends a poor prognosis particularly in pts failing 2 nd-generation TKIs. Cells with BCR-ABL1 T315I mutations are insensitive to 1 st- and 2 nd -generation TKIs, and compound BCR-ABL1 mutations complicate management with all TKIs (including 3 rd-generation ponatinib). Olverembatinib is a novel, potent, 3 rd-generation, orally active BCR-ABL1 TKI with promising activity against CML , largely irrespective of genotype and has a preliminary favorable safety profile.
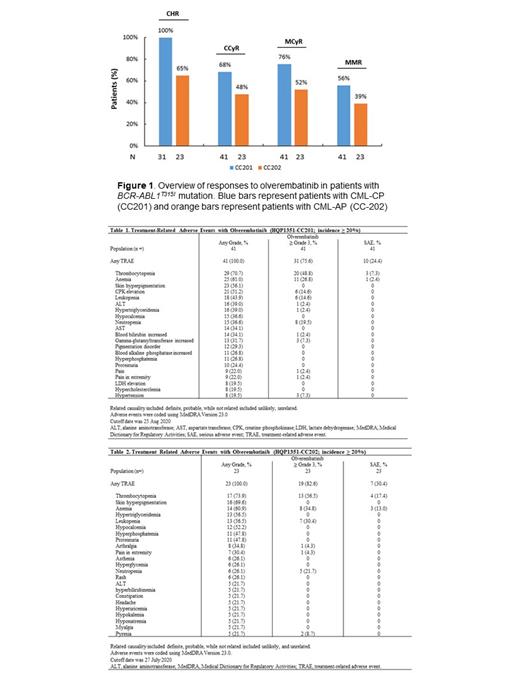
Methods: HQP1351-CC201 and HQP1351-CC202 are Chinese open, single-arm, multicenter phase 2 trials evaluating the safety and efficacy of olverembatinib in adults with TKI-resistant (BCR-ABL1 T351-mutated) CML-CP and CML-CP, respectively. Olverembatinib was administered at 40 mg orally on alternate days for 28-day cycles. The primary outcome measure is major cytogenetic response (MCyR) and major hematologic response (MaHR) by the end of Cycle 12 in CML-CP and CML-AP, respectively. Secondary study endpoints include : complete CyR (CCyR), complete hematologic response (CHR), major molecular response (MMR), progression-free survival (PFS), overall survival (OS), and safety, including treatment-related adverse events (TRAEs) and serious AEs (SAEs).
Results:
Baseline characteristics
Study CC201(CML-CP)
On the study cutoff date of August 25,2020, 41 pts were enrolled, of whom 32 (78%) completed ≥ 12 cycles and 21 (51.2%) were male. The median (range) follow-up was 13 (3.1-16.3) months, age was 47 (22-70) years, and interval from CML diagnosis to first olverembatinib dose was 5.31 (0.6-23.2) years. In all, 32 (78.1%) pts had received ≥ 2 prior TKIs and 9 pts withdrew because of progressive disease (PD), intolerance, or consent withdrawal before Cycle 12.
Study CC202(CML-AP)
On the cut-off date of July 27, 2020, 23 pts were enrolled, of whom 14 (61%) had completed ≥ 12 cycles and 18 (78.3%) were male. The median (range) follow-up was 13.5 (1.4-15.2) months, age was 41 (21-74) years, and interval from CML diagnosis to first olverembatinib dose was 4.96 (0.4-10.2) years. In all, 18 (78.3%) pts had received ≥ 2 prior TKIs, and 11 pts withdrew because of PD or intolerance before Cycle 12.
Efficacy
Study CC201(CML-CP)
After ≥ 12 treatment cycles in pts without responses at baseline, all 31 (100%) experienced CHR (10 other pts had CHR at baseline); 31/41 (75.6%) MCyR; 28/41 (68.3%) CCyR; and 23/41 (56.1%) MMR (Figure 1). The median time to CHR was 1 (95% CI = 1.0-1.9) month, the median time to MCyR was 2.8 (95% CI = 2.8-5.6) months, and the median time to MMR was 6.5 (95% CI = 2.8 to not reached [NR]) months. At 12 months, the PFS rate was 89.3% (95% CI = 73.9%-95.8%), and the OS was 100% (95% CI = 100%-100%).
Study CC202(CML-AP)
After ≥ 12 treatment cycles in pts without responses at baseline, 17/23 (73.9%) experienced MaHR (65.2% CHR and 8.7% no evidence of leukemia [NEL]); 12/23 (52.2%) MCyR; 11/23 (47.8%) CCyR; and 9/23 (39.1%) MMR (Figure 1). The median time to MaHR was 2.8 (95% CI = 1.0-4.7) months, the median time to MCyR was 5.6 (95% CI = 2.00-NR) months, and the median time to MMR was 13.1 (95% CI = 5.6-NR) months. At 12 months, the PFS rate was 74.1% (95% CI = 48.2%-88.4%), and the OS was 91.3% (95% CI = 69.5%-97.8%).
Safety
Study CC201(CML-CP)
Frequent TRAEs (all grades; grade 3-4; SAEs) included thrombocytopenia (70.7%; 48.8%; 7.3%), followed by anemia (61%; 26.8%; 2.4%), leukopenia (43.9%; 17.1%; 0), and neutropenia (36.6%; 19.5%; 0). Common nonhematologic TRAEs (all grades; G3-4) included skin pigmentation (56.1%, 0%) and elevations in creatine kinase (51.2%, 14.6%), ALT (39%, 2.4%) and AST (34.1%, 0) (Table 1). No deaths occurred.
Study CC202(CML-AP)
Common TRAEs (all grades; G3-4; SAEs) included thrombocytopenia (73.9%; 56.5%; 17.4%), anemia (60.9%; 34.8%; 13.0%), leukopenia (56.5%; 30.4%; 0), and neutropenia (26.1%; 21.7%; 0). Common nonhematologic AEs included skin pigmentation (69.6%), hypocalcemia (52.2%), proteinuria (47.8%), hypertriglyceridemia (56.5%), hyperphosphatemia (47.8%), hyperuricemia (21.7%), and arthralgia (34.8%), of which most were grade 1-2 (Table 2).
Conclusions: Olverembatinib was efficacious and well tolerated when administered as monotherapy in pts with TKI-resistant CP-CML and AP-CML and the BCR-ABL1 T315Imutation. Internal study identifiers: HQP1351-CC201-CC202. ClinicalTrials.gov identifiers: NCT03883087 and NCT03883100.
Chen: Ascentage Pharma (Suzhou) Co., Ltd: Current Employment, Current equity holder in publicly-traded company. Niu: Ascentage Pharma (Suzhou) Co., Ltd: Current Employment, Current equity holder in publicly-traded company. Men: Ascentage Pharma (Suzhou) Co., Ltd.: Current Employment, Current equity holder in publicly-traded company. Yang: Ascentage Pharma (Suzhou) Co., Ltd: Current Employment, Current equity holder in publicly-traded company, Other: Leadership and other ownership interests, Patents & Royalties, Research Funding. Zhai: Ascentage Pharma Group Inc.: Current Employment, Current equity holder in publicly-traded company, Other: Leadership and other ownership interests, Patents & Royalties, Research Funding; Ascentage Pharma (Suzhou) Co., Ltd.: Current Employment, Current equity holder in publicly-traded company, Other: Leadership and other ownership interests, Patents & Royalties, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal